Aim:
CD19 chimeric antigen receptor T cell (CAR-T) therapy is a revolutionary treatment for relapsed/refractory (R/R) B-cell hematologic malignancies. However, the safety and efficacy of murine CAR-T cells which have been widely used as commercialized products still need to be improved. Similarly, murine CAR-T encountered the problem that CAR-related immunogenicity existed after the infusion, which led to the failure of the re-infusion of CAR-T cells. As an improved generation of murine CAR-T cells, whether humanized CAR-T therapy can overcome the above shortcomings remains to be explored.
Methods:
In this study, the differences in safety, efficacy, and long-term follow-up results of murine and humanized CD19 CAR-T cells in patients with B-cell malignancies were collected and analyzed. A total of 130 patients were enrolled, including 35 patients with murine CAR-T and 95 with humanized CAR-T cells (NCT 02965092, NCT 04008251).
Results:
The proportion of patients with cytokine release syndrome (CRS) in the murine and humanized groups was 54.3%(19/35) and 61.1%(58/95), respectively. A significantly higher proportion of patients suffered from severe CRS in the murine group than that in the humanized CAR-T group (17.14% vs. 7.4%, P=0.0233), and one patient in each group died of Grade 5 CRS. The incidence of grade 1-2 Immune effector cell-associated neurotoxicity syndrome (ICANS) was 11.4% (murine: 4/35) and 5.3% (humanized: 5/95), but high-grade ICANS was not observed.
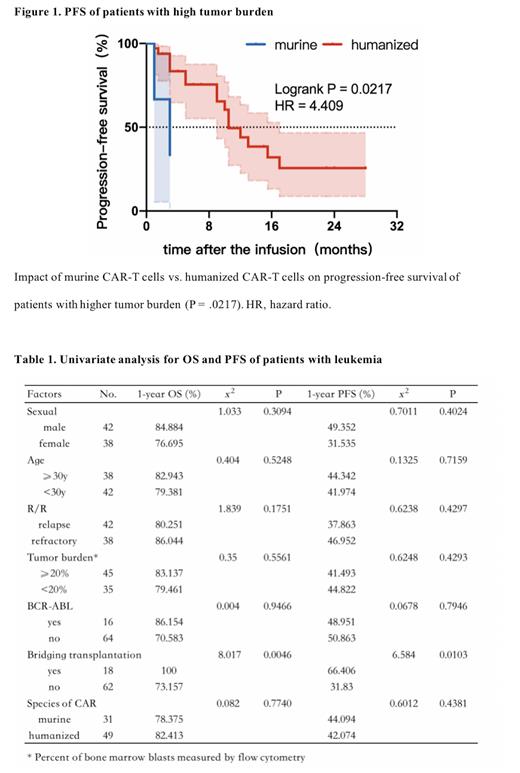
Among patients receiving murine CAR-T cells, 80% achieved objective response (OR), 71.43% achieved complete response (CR) and the CR rate of patients with leukemia was 74.19%. The OR rate and CR rate of patients in the humanized group were 75.79% and 63.16%, respectively, while the CR rate of patients with leukemia receiving humanized CAR-T cells was 89.58%. The median follow-up time of patients in the murine and humanized groups was 7 months (0.6-75 months) and 5.5 months (0.5-34 months), respectively. The median progression-free survival (PFS) of patients with murine CAR-T cells was 11 months and that of patients with humanized CAR-T products was 12 months. Both of the median overall survival (OS) were not reached. Among the 48 patients with a bone marrow burden over 20% at baseline, humanized CAR-T therapy was associated with a higher OS rate (84.64% vs. 59.26%, P=0.1479) and a significantly improved PFS (43.94% vs. 33.33%, P=0.0217, Figure 1).
Bridging transplantation was an independent factor in prolonging OS (x 2=8.017, p=0.0046) and PFS (x 2=6.584, p=0.0103) of patients with leukemia. Neither species of chimeric antigen receptor nor common risk factors such as age, recurrence, bone marrow burden, BCR-ABL fusion gene had significant effect on patients' long-term follow-up outcomes (Table 1). Four patients received CAR-T therapies more than once. Three of them still achieved varying degrees of long-term remission after multiple humanized CAR-T infusions. However, one patient relapsed as soon as one month after his second infusion of murine CAR-T cells.
Conclusion:
Results indicate that humanized CAR-T therapy showed better safety and durable efficacy, especially in patients with higher tumor burden in bone marrow. Moreover, it could overcome immunogenicity-induced CAR-T resistance, providing treatment options for patients' failures of CAR-T therapies.
Disclosures
No relevant conflicts of interest to declare.